Eye Treatment
Cataract surgery
Cataract surgery technique has undergone several changes in last few decades. Newer techniques makes it faster, better and hence better visual outcomes. Main focus has been on decreasing the size of incision to enhance the recovery and changes in quality of IOL.


1. What Is Cataract?
Clouding of the natural lens of the eye preventing light from passing clearly through it, causing loss of vision, usually a result of ageing. But can also occur due to various systemic and ocular diseases like diabetes, uveitis etc.
2. How it can be treated ?
Surgery is the only option for cataract. Cataractous lens is removed and then replaced by an artificial intraocular lens either rigid or foldable IOLs.
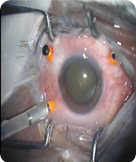
Phacoemulsification :
This is the technique where the cataractous lens is dissolved and aspirated through a corneal or limbal incision and a special foldable lenses are introduced through the same incision.
Phacoemulsification performed through smallest possible incision ( 1.8.mm) and preloaded folded lens is placed through the same incision. Microphaco is designed to speed the recovery of vision, improve visual outcomes and reduce the restriction on your activities after the surgery.
Since the laser is the cutting tool during the entire surgery, no blades or knives are used during the procedure, also earning it the nomenclature of bladeless cataract surgery. A computer controlled laser is a more precise and a better cutting tool than a hand held blade. For people who have a phobia for blades and needles working on such a delicate system as the human eye, this will come as a welcome relief.
Lasik Laser
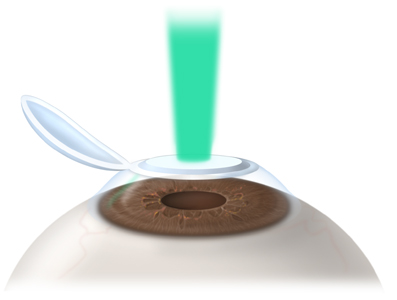 Laser changes the curvature of cornea to correct the spectacle power of eye. The most common types of laser eye surgery include LASIK, SBK, PRK or Bladeless LASIK and the surgeon decides the procedure depending on the spectacle power and the corneal thickness of the patient. Each of the laser eye surgery procedures uses the same special laser, called an "excimer" laser, to reshape the cornea.
Laser changes the curvature of cornea to correct the spectacle power of eye. The most common types of laser eye surgery include LASIK, SBK, PRK or Bladeless LASIK and the surgeon decides the procedure depending on the spectacle power and the corneal thickness of the patient. Each of the laser eye surgery procedures uses the same special laser, called an "excimer" laser, to reshape the cornea.
1. C- LASIK (Laser in Situ Keratomileusis)
LASIK starts with the creation of a thin flap in the cornea. The surgeon uses a motorized blade to make this flap. Once the flap is created, the excimer laser is used to reshape the cornea, which corrects the refractive error and then the flap is deposited back.
2. SBK (Sub-Bowman's Keratomileusis)
SBK is a refractive procedure which creates a thinner flap than standard LASIK.It is has advantage over the standard procedure as it leaves more residual bed in the cornea & hence gives better strength to cornea after surgery. It is the procedure of choice in thin corneas.
3. PRK (Photorefractive Keratectomy)
PRK starts with the removal of a portion of surface of the cornea or epithelial tissue. There is therefore no need for flap creation, and the removed tissue grows back. Some patients are better candidates for PRK eye surgery than for LASIK (for instance, people with thin corneas). Once the epithelium is removed, a laser is used to reshape the cornea.
However, compared to SBK , the PRK recovery period is a bit longer and is little more uncomfortable to the patient.
4. Bladeless LASIK ( Femto or i- LASIK)
The surgeon uses a laser to make flap & there is no use of motorized blade. The laser is considered more desirable by some doctors because of its precision, such as fewer visually significant complications; however, all-laser LASIK costs a bit more than LASIK that uses a blade. Once the flap is created, the excimer laser is used to reshape the cornea, which corrects the refractive error.
Who is a candidate for laser eye surgery?
Laser eye surgery is recommended for people aged 18 or older. It's important to have a record of stable vision for at least a year before having laser eye surgery. Additional criteria like normal thickness of cornea and retinal evaluation must be met to be a candidate for laser eye surgery.
INTACS (Intra corneal ring segments): INTACS is face of modern technology for Refractive Correction. It is useful in low myopia -1.0D to -3.0D and in cases of keratoconus. However, in low myopia the choice of refractive correction is Lasik. Only when patient is not eligible for LASIK, intacs is preferred.
INTACS is face of modern technology for Refractive Correction. It is useful in low myopia -1.0D to -3.0D and in cases of keratoconus. However, in low myopia the choice of refractive correction is Lasik. Only when patient is not eligible for LASIK, intacs is preferred.
In keratoconus ,Intacs act by centering the cone, reducing the cylinder power and improving the quality of vision (by reducing aberration at the level of cornea). Patient of keratoconus can under-go Intacs with or without C3R procedure but it is preferable to do both the procedure at the same sitting. There may or may not be small amount of residual power after intacs which can be corrected by wearing specs or contact lenses. The tolerability of contact lenses is much better after INTACS as it flattens the cornea and the quality of vision for keratoconus patient after Intacs is much better ever after wearing specs.
Patient of keratoconus can under-go Intacs with or without C3R procedure but it is preferable to do both the procedure at the same sitting. There may or may not be small amount of residual power after intacs which can be corrected by wearing specs or contact lenses. The tolerability of contact lenses is much better after INTACS as it flattens the cornea and the quality of vision for keratoconus patient after Intacs is much better ever after wearing specs.
ORTHOKERATOLOGY (Corneal remoulding/Reshaping): Orthokeratology is a novel treatment for spectacle removal without surgery in myopic patients. It involves wearing specially designed contact lenses at night to mould corneal shape .In the morning, the patient can take off the contact lenses and enjoy good vision for the whole day.
Orthokeratology is a novel treatment for spectacle removal without surgery in myopic patients. It involves wearing specially designed contact lenses at night to mould corneal shape .In the morning, the patient can take off the contact lenses and enjoy good vision for the whole day.
This treatment is very useful for patients who want to get rid of Spectacles but are wary of surgery or are unfit for Lasik. It has no age limit and can be prescribed for distance correction to patients more than 40 years of age also. Studies have shown that it can also be prescribed to children more than 10 years of age to arrest the progression of myopia considerably.
Computer Vision Syndrome (CVS)
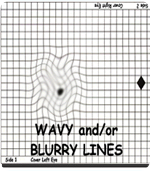
Computer vision syndrome (CVS) is a temporary condition resulting from focusing the eyes on a video display for protracted, uninterrupted periods of time.
Anyone who uses a computer for
prolonged periods — whether on the job, at school or at home for enjoyment — is at risk for headaches, burning eyes, a stiff neck and other symptoms that comprise computer vision syndrome (CVS).
These symptoms can be further aggravated by improper lighting conditions (ie. bright overhead lighting or glare) or air moving past the eyes (e.g. overhead vents, direct air from a fan).
Symptoms

![]() Headaches
Headaches
![]() Blurred vision
Blurred vision
![]() Neck pain
Neck pain
![]() Redness in the eyes
Redness in the eyes
![]() Fatigue
Fatigue
![]() Eye strain
Eye strain
![]() Dry, irritated, burning eyes
Dry, irritated, burning eyes
![]() Double vision
Double vision
![]() Polyopia
Polyopia
![]() Difficulty refocusing the eyes
Difficulty refocusing the eyes
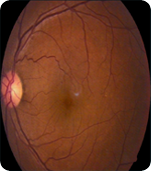
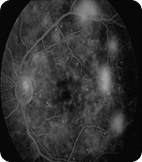
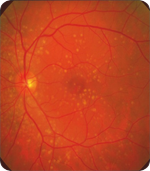
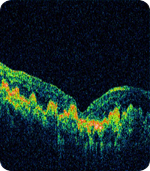
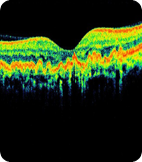
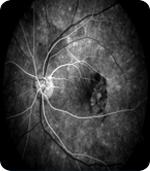
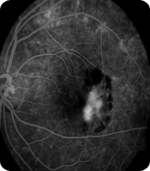
Diabetic Retinopathy
Patient might be asymptomatic or presents with blurring of vision/floaters or sudden loss of vision.
Types of Diabetic Retinopathy
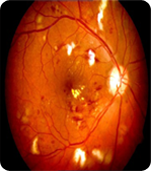
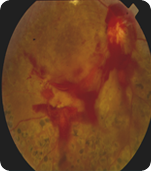
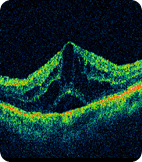
Investigations Required:




Treatment Options :
Aim of treatment remains stabilization of vision and to prevent further progressiona and related complications.








Recommended Diabetic retinopathy screening schedule for diabetic retinopathy patients.
Diabetic Retinopathy : Recommended Follow –up schedule
Status Retinopathy Follow-up (month)
No retinopathy or micro aneurysm only 12
Mild/Moderate NPDR without macular edema 6-12
Mild/Moderate NPDR with macular edema , not clinically significant 4-6
Mild/Moderate NPDR with CSME 3-4
Severe/Very Severe NPDR 3-4
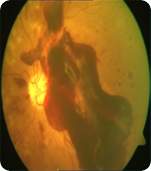
Age Related Macular Degeneration ( ARMD/CNVM) :
Presentation:



Risk Factors :
Types of ARMD:
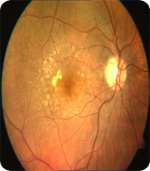

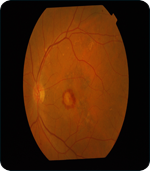
Investigations Required:
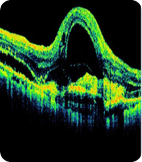
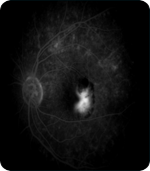
Treatment Options :



managed by drspchaudhary

